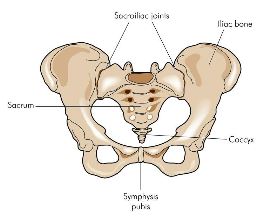
Sacroiliac Joint Dysfunction – the essentials
Please note –
the following does NOT discuss inflammatory sacroiliac joint pathology (sacroilitis)
Presentation
 Females >> Males (most commonly aged 45 to 65)
Females >> Males (most commonly aged 45 to 65)- Nulliparous or exclusively c-sectioned women are less frequently affected.
- Consider in patients with ‘soft’ S1 radicular symptoms or persistent gluteal pain without convincing evidence of impingement on imaging.
- Consider in patients with a history of failed medical or manual treatments.
- There is no need to image the SI joint (unless you are considering an inflammatory joint arthropathy). X-rays, CT’s MRI or bone scans provide no useful information to enable the diagnosis or treatment of sacroiliac movement disorders. Imaging may be of assistance to exclude other lumbosacral pathologies that present similarly or co-exist with SI dysfunction.
- Consider in patients with lumbar fusions (Surgical or anatomical – particularly L5/S1).
- Consider in both genders with significant leg length discrepancy or history of significant pelvic trauma (e.g. motor bike accident).
- Patients may give a poor history or a vague summary of their symptoms.
- Prolonged sitting is a common aggravating factor but an absence of this feature does not exclude the diagnosis.
- Over-diagnosed by physiotherapists and under-diagnosed by doctors.
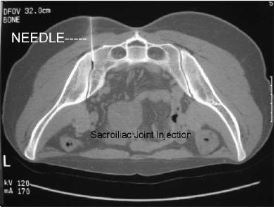
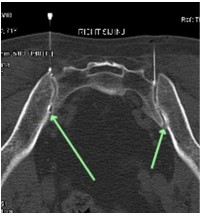
- Confirmation of the diagnosis can only be made by the patient reporting pain relief following an intracapsular SI joint injection – a very difficult injection to perform (even under CT guidance) and one that is frequently mis-reported as ‘accurate needle placement’. Doctors should review all images of SI joint injections to confirm the procedure has been performed correctly by the radiologist.
- A ‘successful’ diagnostic injection will likely provide only short-term relief of the patient’s symptoms (6 to 12 hours – a small percentage report relief lasting several days or weeks). It is essential that:
a) False positives are excluded (usually due to injecting too much fluid volume into the joint),
b) False negatives are excluded (due to placement of the needle not being within the joint capsule – very common) and
c) The patient is advised to deliberately and vigorously perform activities and postures that normally exacerbate their symptoms immediately following the injection (hourly for 6 to 12 hours) and then continue to monitor and record a ‘pain diary’ for one week after the injection.
Clinical findings
- Tenderness over the SI margin – this alone does NOT confirm the diagnosis. Push firmly over the superior and inferior margins of the joint ensuring to direct pressure over the ilium (not the sacrum) in a posterior-to anterior direction.
- Gluteal, PSIS or lumbar pain with prolonged sit or stand. Differentiate from cluneal nerve involvement.
- Chronic, unilateral/asymmetrical lumbar or gluteal pain (but can be bilateral and symmetrical).
- Usually no causative event although chronic lumbar pain from other sources may precede the onset of SI joint pain. Acute presentations (although rare) can present very much like lumbar disc pathologies – imaging may be of benefit to differentiate.
- Tenderness inferior to the PSIS and medial iliac crest (medial gluteal tendonoses)
- Patients will often have a preferred ‘side’ upon which they weight bear whilst sitting or standing.
- Imaging, including bone scan, rarely reveals SI issues (not so in sacroilitis)
- Poor response to oral SAIDs or NSAIDs.
- Short-term and incomplete relief with manual therapies.
Definitive diagnosis is obtained by local anaesthetic injection into the joint. The addition of steroid rarely improves outcomes but is worthy of inclusion. If concerns for bilateral SI dysfunction exist, each side should ideally be injected at least one week apart.
NOTE – relief of symptoms following this procedure is nearly always very short lived (usually 6 to 12).
It is vital that a patient keep a very accurate pain-diary in the hours and days immediately after their injection.
Patients should be provided with an hourly pain-diary to complete and rate their pre and post procedure pain levels out of 10. (“Better” “same” or “worse” is not sufficient)
Diagnosis
- Asymmetrical iliac movement with lumbar flexion or extension is suggestive but not clinically sensitive enough to diagnose SIJ dysfunction and such asymmetry in movement is extraordinarily hard/impossible to assess in obese patients.
- Sacroiliac compression test, sacroiliac distraction test, thigh thrust test, sacral thrust test and Gaenslen’s test are quick tests. Pain reproduction on 3 or more of these is highly diagnostic for SI joint dysfunction.
- Accurate sacroiliac injection (under CT guidance) is the gold-standard. Be warned – this is usually a painful injection and radiologists (who are likely pressured by a patient in pain) frequently ‘miss’ the joint. Doctors – ask the radiologists to provide ALL imaging so you can confirm accurate needle placement. Ensure contrast is used and that infiltration/spill of contrast can be seen into the anterior joint.
Differential diagnoses
- S1 radiculopathy
- Medial gluteal tendonoses (often co-exists)
- Pelvic congestion syndrome/pelvic vein incompetence (pelvic CT venogram/transvaginal doppler)
- L5/S1 facet arthropathy
- L5/S1 spondylosis
- Ankylosing spondylitis (other inflammatory arthropathies)
- Trochanteric bursal ‘syndrome’.
- Piriformis syndrome – a rare diagnosis.
Physiotherapy treatment
Physiotherapy intervention is most effective in early presentations of SI dysfunction (where symptoms have been present for less than 3 months). Beyond this time physiotherapy treatment is likely to be prohibitively expensive (in excess of 6 treatments) and the rehabilitation required has an extraordinary low compliance rate.
Physiotherapists are often the first to diagnose SIJ dysfunction (and frequently over-diagnose it). Treatment may include:
- Release of proximal gluteal musculature. Usually done very poorly by physiotherapists resulting in painful treatments that leave the patient feeling bruised. Such treatment is fundamental to recovery and should be painless.
- Lumbar and sacroiliac joint mobilisations.
- Appropriate sacroiliac brace fitting
- Core, gluteal strengthening and pelvic floor exercises have some weak evidence behind them (remember compliance is poor and it is usually unreasonable to expect third-party insurers to fund this type of rehabilitation.
Note – there is no evidence to support the use of ultrasound for ANY pathology.
Be wary of the therapist who advocates expensive rehabilitation programmes. The evidence to support efficacy is poor and patient compliance is poorer.
Medical Treatment
- SI joint steroid injection –request that long-acting local anaesthetic be used in combination with long-acting steroid (eg Depo-medrol)
It is VITAL that patients keep an hour-by-hour ‘pain-diary’ following this procedure. Only short-term relief (hours or days) is expected. The aim is to diagnose the pathology and justify rhizotomy (strip ablation), prolotherapy or SI fusion.
- SI joint rhizotomy/radio-frequency ablation (RFA) L5, S1, S2 and S3 – This is a difficult procedure (compared to facet rhizotomies) and is best followed up (6 weeks later) with steroid injection to the medial gluteal tendons/medial iliac rim and gluteal release. Chronic SIJ dysfunction frequently has gluteal tendonopathic pathology (medial and lateral tendons) +/- trochanteric bursitis. Hence rhizotomy alone is unlikely to provide full resolution of symptoms.
Prolotherapy treatments
- Of the several prolotherapy options available Platelet Rich Plasma shows the most promise for CONFIRMED SIJ dysfunction. Usually two injections are required into the joint, 4 to 6 weeks apart (approximately $500per injection which makes this untenable for most patients). Results take 8 to 12 weeks.
- Hyperosmolar sugar/dextrose solutions can also be injected into the dorsal interosseous ligaments. Injections cost around $75 to $100 (per side). 4 to 6 injections are required around 4 weeks apart. Injections are uncomfortable and post procedural pain may last for up to one week.
Surgical treatments
SI joint fusion is successful but rarely performed – even minimally invasive approaches are complex high-risk surgeries with 9 to 12-month recovery.
Take home message
- Over-diagnosed by physiotherapists and under-diagnosed by doctors.
- Physiotherapy is helpful to treat concomitant sources of lumbar pain
- Local anaesthetic (+/- steroid) is the gold standard for diagnosis – will provide short-term relief only.
- An accurate pain-diary following SI steroid/long-acting local anaesthetic injection is vital.
- Radiologists OFTEN do not place the injection within the join so it is vital that the GP view and confirm an accurate injection.
- Imaging is a poor diagnostic indicator.
- Extremely rare in males and nulliparous women.
- Work with a Pain Physician to coordinate rhizotomy and follow up injections and physiotherapy. Quality after-care is essential to achieve full recovery.
- Consider this diagnosis in mothers with persistent lumbar (+/- radicular) pain and benign imaging.
- Treat early presentations (less than 12 weeks) aggressively. Short-term, high-dose oral corticosteroids, NSAIDs and physiotherapy together often work extremely well in this period.
To discuss your lumbar pain with one of the doctors at Kingsley Medical please be sure to bring ALL imaging to your consultation. It is important that you understand our fees before making a booking. Click here for an outline of our fees. Please understand that Kingsley Medical is not a bulk billing clinic. Please do not ask to be bulk billed.
Please prepare for your consultation by reading our guidelines here.