Frozen Shoulder
 Frozen shoulder (also called “adhesive capsulitis”) is a common condition that results in the progressive stiffening of the shoulder joint. It is more commonly experienced by women and most frequently seen in the 40 to 60 year age group. It is characterised by a decreased range of movement of the shoulder in most or all directions and by diffuse tenderness around the joint margins. The key to successfully managing frozen shoulder relies on an accurate diagnosis and a precise ‘staging’ (discussed below). This is not always easy. Many other conditions can mimic the initial symptoms of frozen shoulder and may in fact co-exist.
Frozen shoulder (also called “adhesive capsulitis”) is a common condition that results in the progressive stiffening of the shoulder joint. It is more commonly experienced by women and most frequently seen in the 40 to 60 year age group. It is characterised by a decreased range of movement of the shoulder in most or all directions and by diffuse tenderness around the joint margins. The key to successfully managing frozen shoulder relies on an accurate diagnosis and a precise ‘staging’ (discussed below). This is not always easy. Many other conditions can mimic the initial symptoms of frozen shoulder and may in fact co-exist.
Your doctor or physiotherapist will assess your shoulder for damage to the rotator cuff muscles, bursitis (of which there are several), arthritis and problems with the cervical spine which may be referring pain to the shoulder. Additionally, your doctor will also assess the sternoclavicular (SC) joint and the acromioclavicular (AC) joint for problems that can present with similar symptoms. Additional differential diagnoses for frozen shoulder include joint infection, joint degeneration (glenohumeral, AC and SC joint) as well as Pancoast’s tumour. Your doctor will exclude these diagnoses in order to confirm frozen shoulder.
Frozen shoulder is a frustrating problem for both patient and doctor. Left untreated, most cases of frozen shoulder will fully recover within 18-36 months. In fact, even with treatment (medical or physiotherapy) the duration of the affliction is unlikely to change significantly. The aim of treatment is to accurately diagnose the condition and its pathological staging (discussed below). Treatment aims to reduce the loss of joint movement so that some functional capabilities will remain. This may sound a bit like ‘damage control’ but it can make considerable difference to the patient’s lifestyle and vocational capabilities during the recovery period.
What causes frozen shoulder?
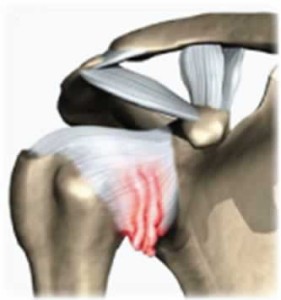
The cause of frozen shoulder is not fully understood. It can develop spontaneously (without any obvious cause) or can develop following shoulder trauma, prolonged immobility of the arm (following a fracture or surgery) or concomitantly with other shoulder pathologies. Thickening and contracture (tightening) of the shoulder capsule is the end result and it is this that brings about a reduced range of movement in the joint. Frozen shoulder is more commonly seen in people with diabetes, thyroid disorders as well as Parkinson’s disease and cardiovascular disease. It may also occur in people without systemic illness or autoimmune diseases.
How is frozen shoulder diagnosed?
The diagnosis of frozen shoulder can usually be made on clinical presentation alone – taking a good medical history and performing a thorough physical examination. Imaging such as x-ray, MR or bone scans may be suggested to rule out other diagnoses or to confirm the presence of co-existing pathologies for which alternate treatments may be available.
Staging frozen shoulder.
Having established the diagnosis it is then necessary to ‘stage’ the condition. Frozen shoulder progresses through 3 “stages” each one usually lasting between 6 to 9 months.
The first stage (often called a “freezing shoulder”) is defined by worsening pain and deteriorating movement of the shoulder. The aim during this stage is to minimize pain and preserve as much range of movement as possible. Aggressive manual therapy or exercise can worsen symptoms so it is vital that you provide your doctor and physiotherapist with feedback about your response to treatment. If improvements in range and/or pain are not readily forthcoming during this period, cease physiotherapy and concentrate solely on the home exercises that you will be given. Oral analgesia or shoulder injections may also be helpful (see below).
The second stage (often called the true “frozen shoulder”) is effectively a plateauing of symptoms. It does not necessarily mean that the shoulder will be left completely immobilised but rather that the deterioration (reduction in range or worsening of pain) will have ceased. Again, physiotherapy techniques to loosen the shoulder joint, AC and SC joints as well as the cervical spine and muscles around the shoulder may be able to improve symptoms during this period. Again, if improvement is not obvious and immediately forthcoming (within 1 or 2 consultations) it is best (safest and cheapest) to stick with a home mobility and strengthening programme. This second stage is often the shortest of the three stages. Injections are usually most beneficial in this stage.
The third stage (a “thawing shoulder”) begins at the time when improvements in range and reductions in pain begin to occur. This is the time in which manual physiotherapy interventions are most effective. Manual joint and muscle release techniques, although uncomfortable, can considerably improve symptoms. In most cases, one or two consultations every 1 to 2 months is all that is required. Remember, if improvement is not significant with these treatments, discuss it with your physiotherapist. This allows for your treatments to be adapted, intensified or ceased completely if necessary. Your therapist will continue to rely heavily on the feedback you give them following each treatment.
Many patients fall into the cycle of continuing with regular (and costly) physiotherapy treatments which do little more than babysit the injury whist it recovers on its own. If you do not feel you are getting substantial benefit from treatment, cease. Remember, frozen shoulder is a problem that will resolve by itself in due time. Physiotherapy simply aims to punctuate bursts of improvement during the natural course of the pathology, reduce the likelihood of secondary shoulder and neck problems and facilitate daily function of the arm.
Medical management options for treating frozen shoulder.
The severity of frozen shoulder can vary greatly from patient to patient. Some people require little more than oral analgesics or anti-inflammatories to assist them through their recovery period. Others may require corticosteroid injections or manipulation of the shoulder joint under general anaesthetic. Hyperdilation (also called hydrodistension or hydrodilation) involves injecting the shoulder joint with saline to expand and stretch the joint capsule. The best outcomes are achieved when this is administered with a corticosteroid injection.
Corticosteroid injections (into the glenohumeral joint) OR hydrodistension (without corticosteroid) rarely produce significant outcomes unless performed concomitantly.
For a full list of our fees and services click here.
To make an online booking with one of our doctors click here.